
→ Click “Fullscreen” below for the best reading experience :).
→ After you have had a read, feel free to download your eBook by clicking the download icon in the top right corner of the document.
Insights from ‘The Lancet’ 2018 global review of the management of low back pain:
⇒ AGE
It’s no secret that your risk of back pain increases as you age, with the first episode of back pain likely to strike around ages 30 – 50 years. This may increase with normal age related changes, however, there are many things that can be done to reduce the risk, and alleviate the symptoms of low back pain as you age.
⇒ FITNESS LEVEL
Individuals with reduced physical fitness are more likely to present with low back pain. In fact, studies show1, engaging in strength training or walking are effective at reducing lumbar pain and improving function.
⇒ WEIGHT AND BODY COMPOSITION
Sudden weight gain, or being overweight increases the mechanical load on your back and is strongly associated with low back pain.
⇒ GENETICS
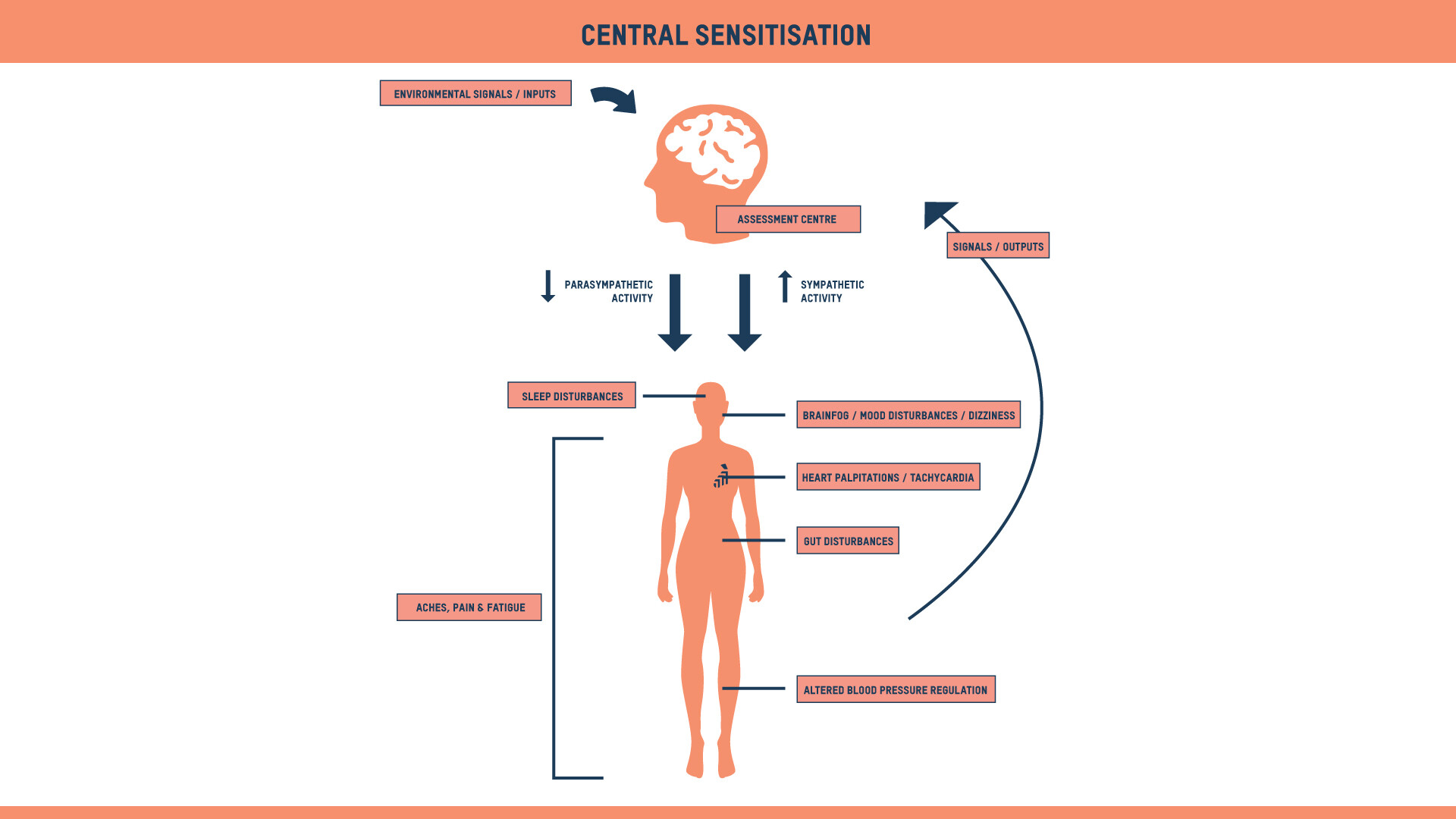
Sudden weight gain, or being overweight increases the mechanical load on your back and is strongly associated with low back pain. Some people are also genetically predisposed to pain conditions and central sensitisation (see diagram below).
⇒ OCCUPATION
⇒ MENTAL HEALTH
⇒ PREGNANCY
⇒ ACUTE LOW BACK PAIN
⇒ CHRONIC LOW BACK PAIN
On occasion, back pain may even be caused by other underlying conditions such as:
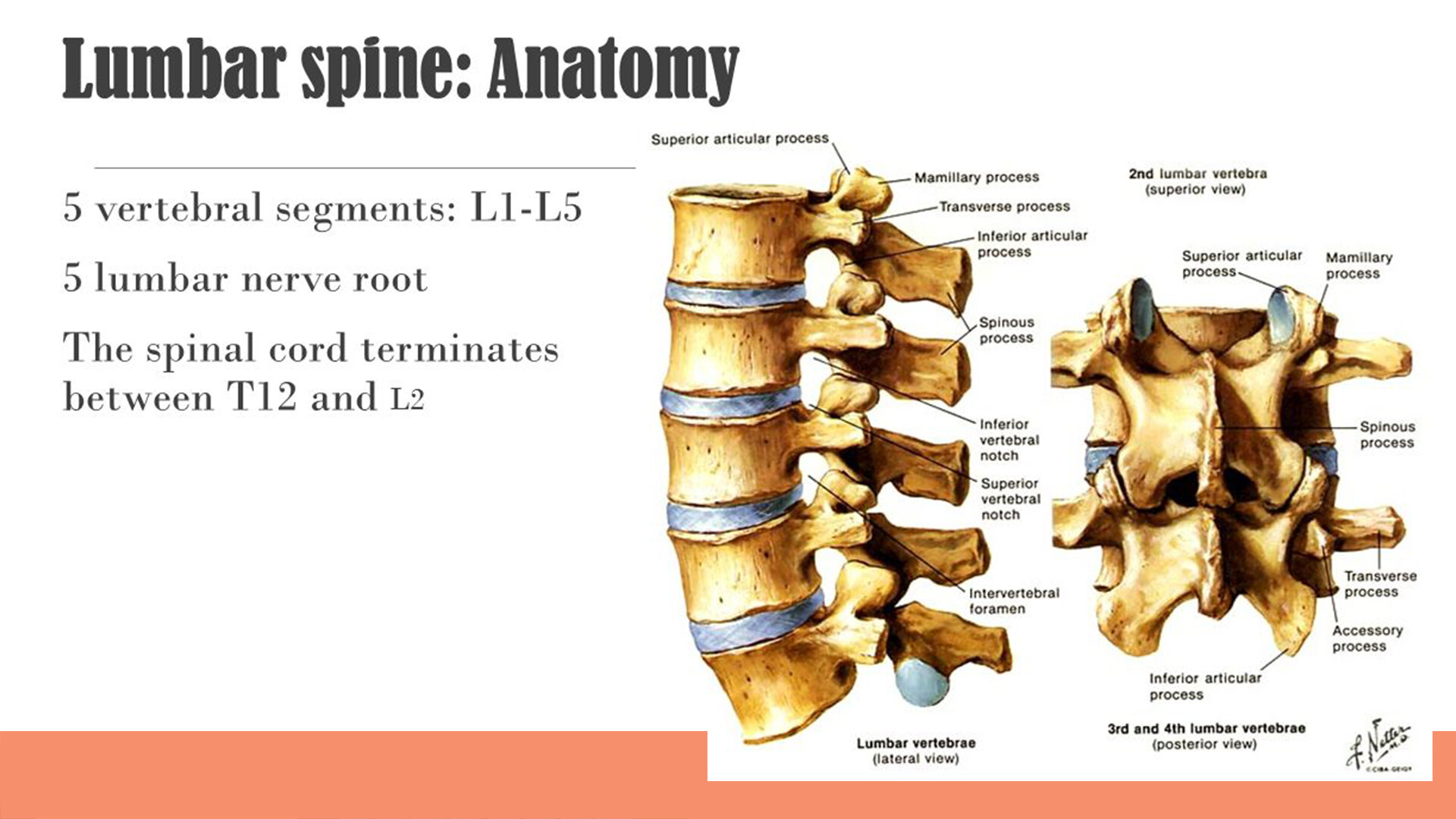
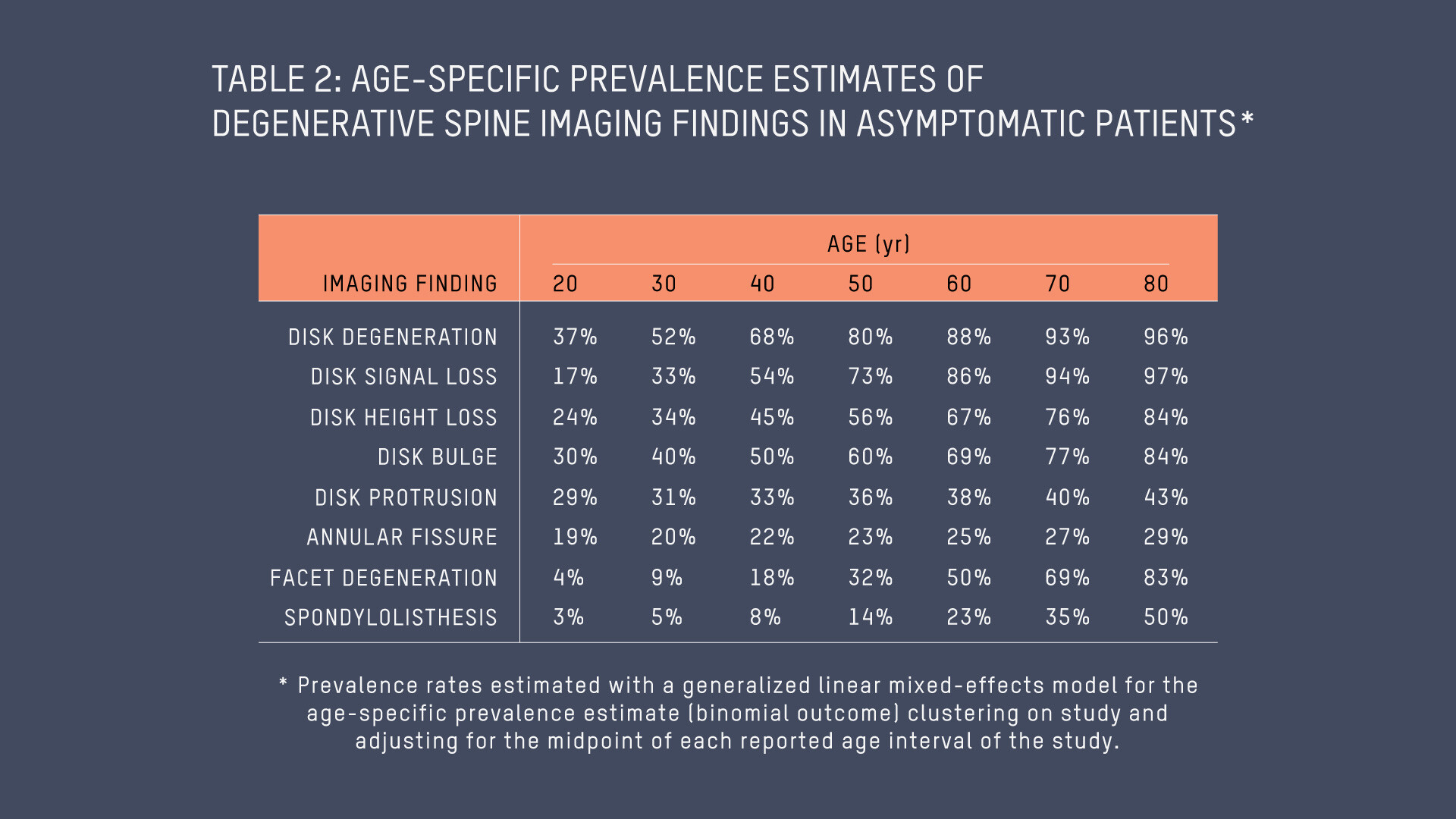
Low back pain can be diagnosed with a thorough assessment from a skilled physiotherapist. As first contact practitioners, you do not require a referral from a GP or specialist to attend. A physiotherapist can not only diagnose, but treat, and provide exercises, education and lifestyle modification to assist in symptom reduction and elimination. Diagnosis requires a combination of verbal questioning and hands on assessment. This is done to quantify range of motion restrictions, strength deficits and any alterations in movement patterns or coordination. As part of your diagnosis, your physiotherapist should include questions about your lifestyle history. This will help them to understand you as a person, how your back pain is affecting your life and the many thoughts and beliefs you may have regarding your back pain and its impact on your quality of life. If scans or imaging are required to assist with your diagnosis, your physiotherapist can refer you for imaging and can interpret
⇒ Read more about back pain exercises in our blog: What are the best exercises for low back pain?
⇒ TOP TIPS:
⇒ TOP TIPS: